What are the main features of the Spanish Preliminary Draft Law on Medicines and Medical Devices?
Published on 28th May 2025
Recent challenges faced by the health sector have led to a comprehensive reform of pharmaceutical legislation in Spain, aligning the system with evolving healthcare demands
A decade after the approval of the Royal Legislative Decree 1/2015 of 24 July, which established the revised text of the Law on Guarantees and Rational Use of Medicines and Medical Devices, the Council of Ministers has now introduced the Preliminary Draft Law on Medicines and Medical Devices.
The primary objectives of this legislative reform are to adapt the system to new pharmaceutical policy challenges, accommodate disruptive scientific advancements, enhance measures for rationalising pharmaceutical spending, promote the rational use of medicines, and implement lessons learned from the pandemic experience.
Some of the key features of the new Preliminary Draft Law are as follows:
Prescription by active ingredient
The new regulatory text stipulates that prescriptions for medications within the National Health System (NHS) must be written using the official Spanish name of the medicine or, if none exists, the international non-proprietary name of the active ingredient. This approach aims to promote the rational use of medications and contribute to the sustainability of the health system.
The Spanish Agency for Medicines and Health Products (AEMPS) will create standardised groupings of equivalent medications. This will enable patients to choose between lower-priced and higher-priced options, paying the difference if they select the more expensive medicines. Exceptions will be made for chronic conditions, vulnerable patients, individuals with adherence issues, and medications classified as non-substitutable by the AEMPS.
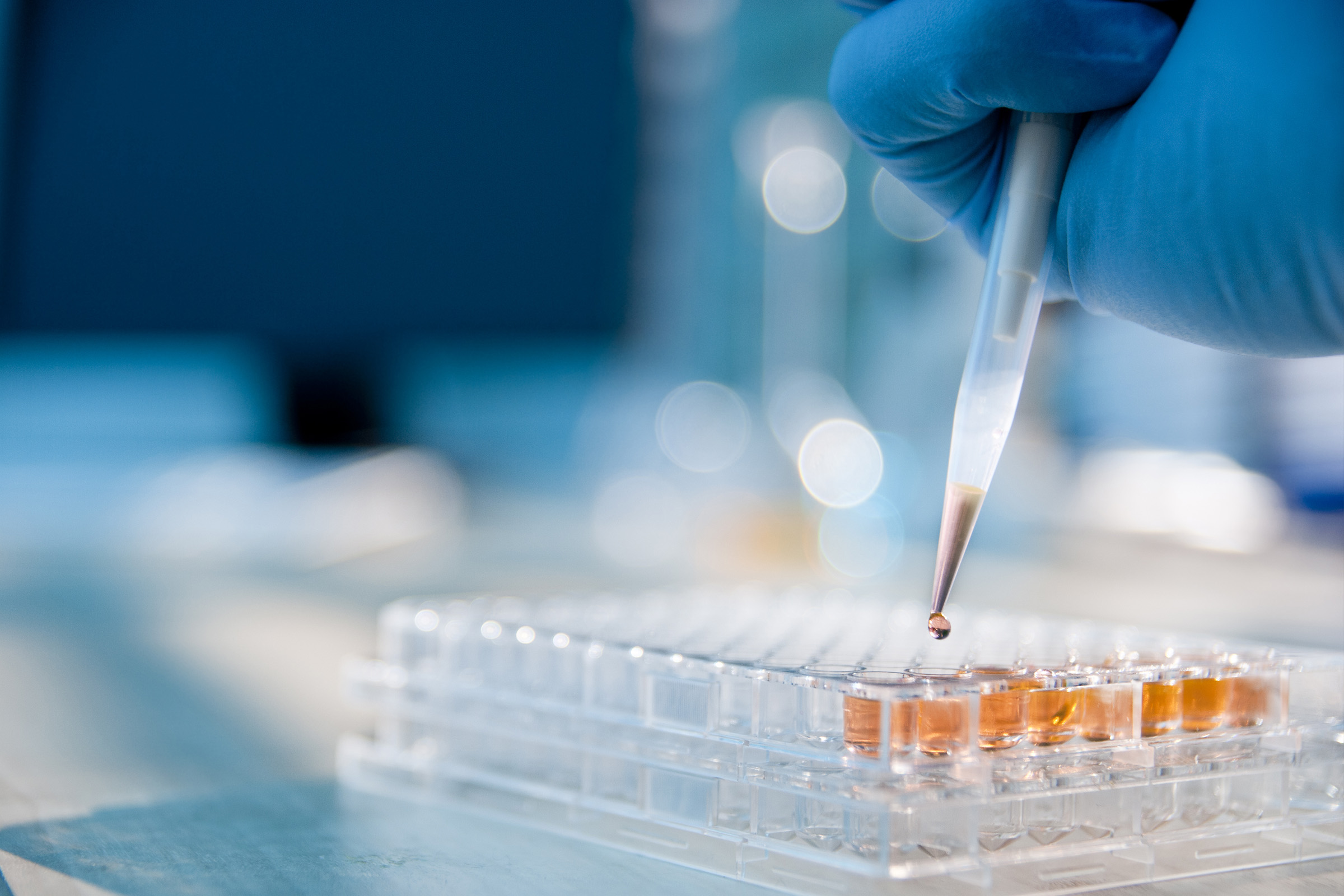
Early, conditional and provisional access to medicines
To improve early access to medicines that significantly affect individuals' health, the new regulation introduces provisions for the accelerated, conditional or provisional inclusion of new drugs or new indications for existing medicines.
This is applicable if these treatments offer alternatives for unmet medical needs and are expected to provide meaningful clinical benefits for patients who cannot afford to delay treatment. Additionally, this process should not result in a greater budgetary impact on the NHS than from a favourable decision on financing.
Extending the competencies of healthcare professionals
The new regulation aims to allow nurses and physiotherapists to prescribe medications within their areas of expertise.
To enhance the coordination of prescribing and dispensing medications, "Pharmacotherapeutic Coordination Councils" will be established. These will consist of medical professionals, nursing staff, primary care pharmacists and pharmacists responsible for community and hospital pharmacy services.
Health technology assessment
The new regulation includes a chapter that establishes a legal framework for a system to evaluate health technologies. A royal decree is currently being developed.
Health technology assessment offers valuable insights into clinical and non-clinical aspects, helping to situate a particular technology within available alternatives. This process aims to evaluate the potential impact of adopting the technology on the health system. The proposed assessment system is designed to be transparent, participatory, scientific and timely. This is expected to enhance the legitimacy of decision-making.
Changes to the public price and financing system
The reference price system has been replaced by the selected price system, which establishes a price range for medicines financed by the NHS. Medicines exceeding the reference price will receive partial financing.
A joint statement by the leading industry associations indicates that this strategy "will create a natural tendency to reduce prices of off-patent medicines, jeopardising the viability of many drug production lines in Spain and exacerbating existing supply issues."
Medicine supply management
The new regulation emphasises the importance of addressing supply challenges. Laboratories will be required to create plans to prevent disruptions in supply and must inform the AEMPS of any quality or manufacturing issues that arise. Additionally, the regulation introduces a category called "strategic medicines" to ensure that essential products remain available in the market.
The new regulatory text introduces a final provision that amends Law 9/2017, dated 8 November, concerning Public Sector Contracts. This law incorporates the European Parliamentary and Council Directives 2014/23/EU and 2014/24/EU, dated 26 February 2014, into Spanish law. The amendments aim to simplify specific procedures for public procurement of medicines and medical devices. They specifically address medicines that are administered only once and whose payment might be linked to maintaining results over periods longer than five years.
Additionally, the regulation encourages joint purchasing whenever deemed appropriate, both at the national and European levels, while integrating these provisions into the existing pharmaceutical supply system.
A new provision has been introduced for developing a procurement guide that offers recommendations for contracts related to the supply of medicines and medical devices.
Other updates
The new legislation includes major updates in areas such as environmental sustainability, veterinary medicinal products, clinical trial evaluations and the enforcement regime.
Osborne Clarke comment
The reforms proposed in the new Preliminary Draft Law have generated a variety of reactions within the pharmaceutical sector. Following the completion of the public hearing process, there is considerable anticipation for the final version of the text, as well as for other relevant Royal Decrees on topics such as Health Technology Assessment and the procedures for financing and pricing medicines.
Farmaindustria has stated that "medicines should not be seen as a public expenditure item, but rather as an investment strategy. The main objective is to improve population health while supporting the sustainability of the welfare state."
Future updates and developments of the new regulatory text must be monitored to achieve these objectives and evaluate their impact on the health and pharmaceutical sectors.