New regulatory framework established for the medicinal use of cannabis in Spain
Published on 24th October 2025
The decree aims to balance therapeutic access to cannabis with guarantees of quality, safety and health control
The Spanish government has approved Royal Decree 903/2025, establishing a clear legal framework for the medicinal use of cannabis in Spain. This regulation outlines the guidelines for the prescription, preparation and dispensing of standardised cannabis-based formulations intended for therapeutic use.
Until now, cannabis use for medical purposes has been restricted to exceptional authorisations and lacked a consistent process. The new legislation aims to provide legal and health security, ensure the quality of cannabis preparations and improve patient access to treatments under strict clinical supervision.
Main therapeutic indications
The regulation addresses the necessity of providing a therapeutic option in situations where standard treatments fall short, particularly for patients suffering from refractory chronic pain, severe epilepsy, or spasticity caused by multiple sclerosis.
The regulation does not provide a fixed list of indications. Instead, it refers to the monographs that the Spanish Agency for Medicines and Health Products (AEMPS) will publish in the National Formulary. These monographs will outline, for each case, the conditions of use, prescribing criteria, dosage guidelines and quality standards.
This approach allows for the addition of new indications as scientific evidence and clinical practice advance, while adhering to strict criteria for effectiveness, safety, and medical necessity.
Limits, conditions and controls
The use of medical cannabis is limited to hospitals. It can only be prescribed by specialised medical personnel, who must justify the prescription and perform individualised clinical monitoring to evaluate efficacy, tolerability and any potential adverse reactions.
The use of these preparations should be limited to when no approved industrial medicines are available for the condition being treated or when existing treatments do not provide satisfactory control for the patient.
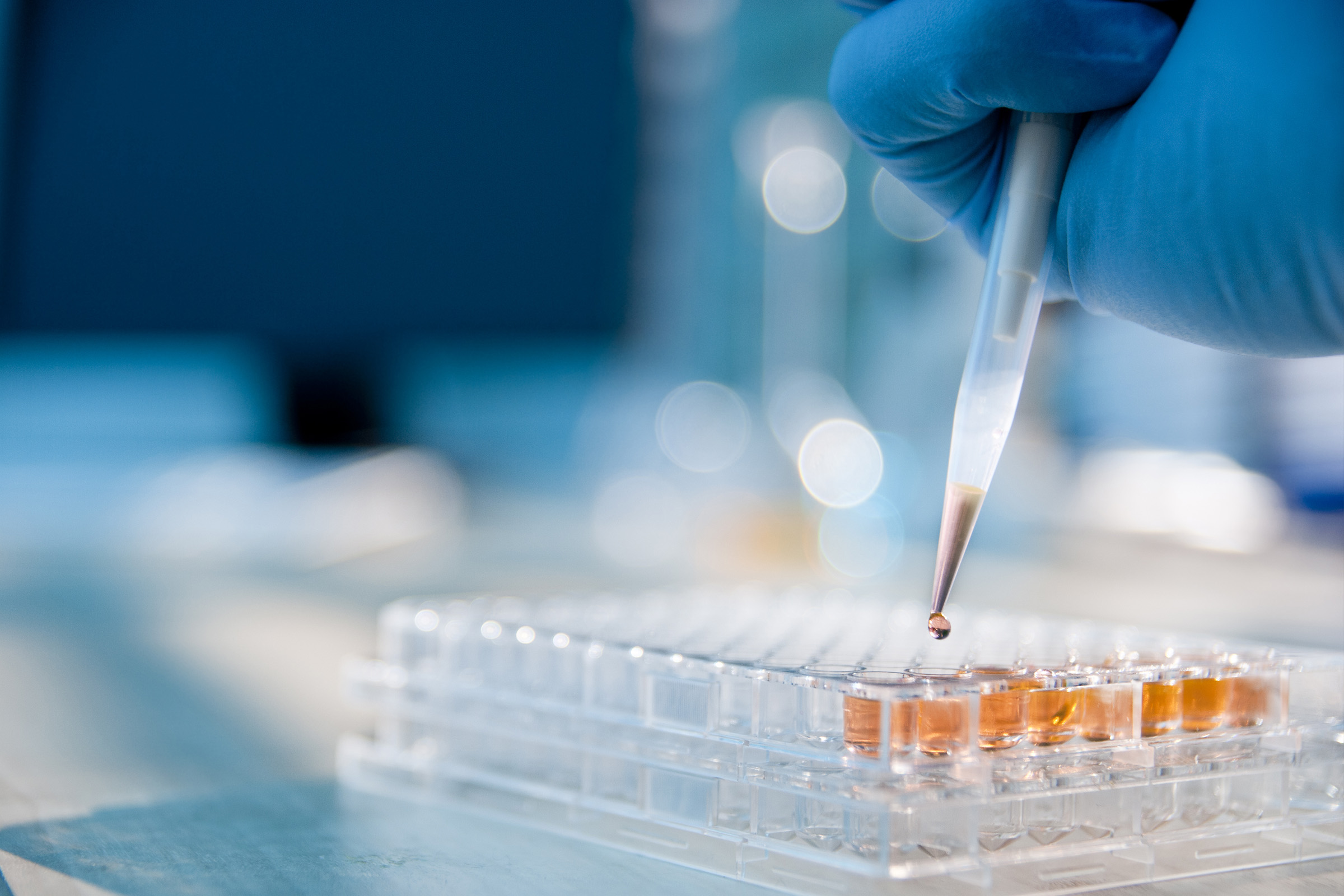
Standardised preparations may only be manufactured by licensed pharmaceutical laboratories. The formulation of these preparations is strictly limited to legally authorised hospital pharmacy services.
The responsibility for dispensing these medications will fall to pharmaceutical care services, working hand in hand with the medical team tasked with monitoring the patient. These medicines will not be available for purchase in pharmacies.
This model ensures traceability and safety in treatments, but it comes with specific operational requirements. Hospital channelling can create barriers for patients who live far from major centres or have limited mobility, complicating their access to care.
Registration, traceability and obligations of preparations
The AEMPS is tasked with creating monographs that outline the conditions of use, dosage, quality, and manufacturing processes for each standardised preparation.
Additionally, a public registry of standardised cannabis products is being established and overseen by the AEMPS. This initiative will allow for the tracking of available formulas and ensure their adherence to European pharmaceutical quality standards.
Pharmacovigilance obligations
Finally, the Royal Decree mandates that physicians must notify the relevant regional pharmacovigilance centre of any suspected adverse reactions they encounter.
Osborne Clarke comment
Royal Decree 903/2025 represents a significant shift in Spanish health policy. This decree establishes the legal framework for the use of medical cannabis within a strictly regulated environment, restricted to hospitals and grounded in scientific evidence. By doing so, Spain aligns itself with other countries like Germany, Italy, the United Kingdom, and Canada.
For patients, it introduces a new treatment pathway in a safe, controlled setting. For healthcare professionals, however, it poses a challenge that demands considerable coordination and oversight.
The success of the regulation will hinge on how well it is implemented in practice. Key factors include the availability and quality of preparations, the clarity of the monographs, hospitals' ability to meet demand, and robust pharmacovigilance to monitor clinical outcomes and safety.